Data integration in healthcare combines and consolidates multiple healthcare data sources — pharma, patient-generated, healthcare provider, wearable apps — into a unified, single data set.
Why does it matter in medtech?
Because for years, medtech growth has been driven by engineering excellence and unit sales of devices. But that model is reaching its end of life.
The future is no longer about the device alone, in medtech it’s about delivering connected healthcare ecosystems where devices, data and software all unite to enable AI-driven insights, patient-centric outcomes and value-based care. Regulatory forces like the FDA’s interoperability mandates, the EU AI Act and the European Health Data Space are accelerating this new era.
At the same time, big tech has entered the arena with formidable expertise in AI, cloud infrastructure, user experience and often a much larger budget. Medtech OEMs need to navigate all of this by owning the integration engine and solving the healthcare data integration challenge. Read our new report below to find out how it's done.
Current challenges facing medtech OEMs
Today, there’s multiple pain points that medtech OEMs need to solve for in order to get ahead.
1. Data fragmentation
80% of healthcare data is unstructured. Data sits siloed within product lines. For example, a patient’s cardiac implant data may live in one system while their diabetes device data is locked in another. That’s because many large medtechs have grown through acquisitions and have disparate IT systems or product platforms that don’t “talk” to each other.
This lack of interoperability makes it nearly impossible to build the holistic digital health strategies that healthcare providers and patients increasingly demand.
Without data integration, medtech OEMs struggle to deliver unified dashboards, integrated care platforms or the kinds of continuous digital services that are fast becoming standard.
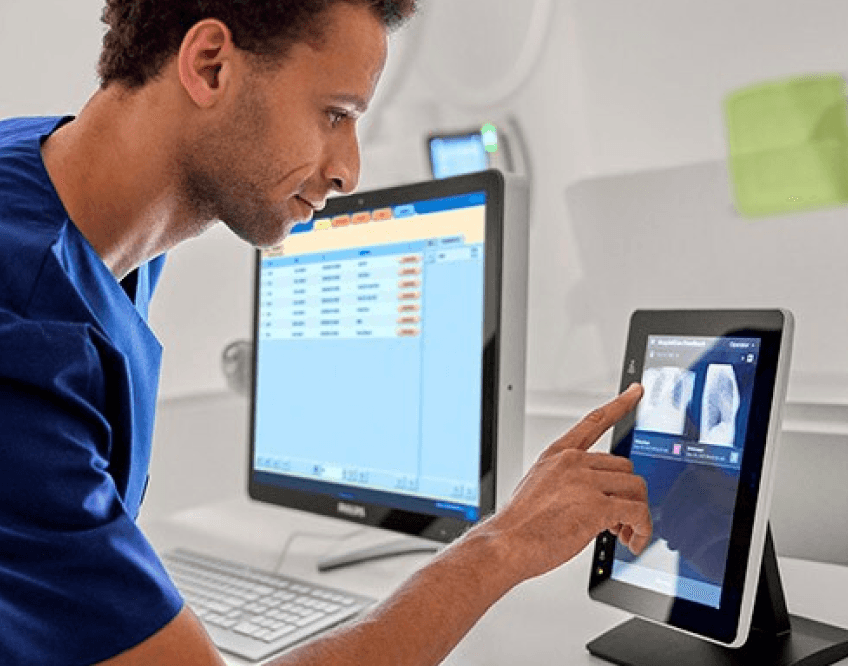
2. Connected services
The pressure to move beyond one-time device sales is mounting. Hospitals, payers, pharma and patients expect ongoing services that deliver continuous value, like remote monitoring, predictive analytics, wearable apps and AI-powered decision support.
Yet designing and scaling these “hook” services has proven difficult for companies whose DNA is rooted in hardware. Building IoT-enabled devices with companion apps doesn’t just require technical infrastructure, it also needs a deep cultural and organizational shift toward software, cloud and agile delivery models.
Healthcare data integration is the prerequisite for making this transformation real. Not to mention it’s also the sticking point holding many organizations back.
3. Regulatory compliance
Compounding the issue are the regulatory and security implications. Every data pathway, API or software update introduces a potential risk, whether it’s a compliance question under HIPAA or GDPR, a cybersecurity vulnerability or a quality system gap.
For medtech companies used to the slower pace of device approvals, adapting to the rapid cycles of digital health can feel overwhelming. And even if they can clear those hurdles, many lack the in-house expertise to drive integration at scale.
Recruiting and retaining top-tier AI engineers, cloud architects and digital product leaders remains an uphill battle when competing with Silicon Valley giants.
4. Market competition
Competitors move quickly. Big tech is already shaping digital health experiences, cited as the leading driver of innovation last year. Startups are partnering directly with providers and payers, bypassing traditional medtech channels.
The competitive question for OEMs is no longer “if” but “how” to compete or collaborate with these players, and whether they can do so without being relegated to the sidelines of the digital health ecosystem
5. Changing consumer demands
Patients and advocacy groups increasingly expect healthcare that’s more personalized and convenient. As consumers gain access to more health data, they’re demanding clearer results and greater control over their care.
For medtech companies, this presents a new challenge: demonstrating outcome-based value.
The central challenge is proving that their devices, combined with digital services, can reduce hospitalizations, boost adherence and deliver measurable clinical and financial benefits for healthcare systems. Achieving and validating these results requires strong data analytics and tools that enable ongoing patient engagement.
Why is data integration important in healthcare?
At the heart of all of these challenges lies a single barrier: without robust healthcare data integration, medtech companies can’t build the connected services, AI capabilities or outcome-driven platforms the market now demands.
Siloed data limits innovation. Legacy systems slow progress. Regulatory risk erodes confidence. And talent shortages make execution harder still. The challenge is clear: medtech OEMs that don’t integrate will struggle to keep up. But those that can will unlock new revenue models, strengthen provider relationships, and position themselves at the center of healthcare’s connected future. How can you achieve that?
What once was a hardware-first market is shifting to an ecosystem-first model. For OEMs, solving the healthcare data integration challenge is more than a defensive play. It opens the door to entirely new business models:
1. Device and data bundles: In this model, devices are packaged with integrated software and analytics dashboards that embed themselves into clinical workflows. That way, OEMs create ongoing subscription revenue while providers gain better patient oversight

2. Platform licensing: Providers pay for interoperability platforms independent of specific devices
3. Third-party marketplaces: Here OEMs open APIs that allow startups and partners to build add-ons like AI diagnostics, digital twins and remote monitoring apps
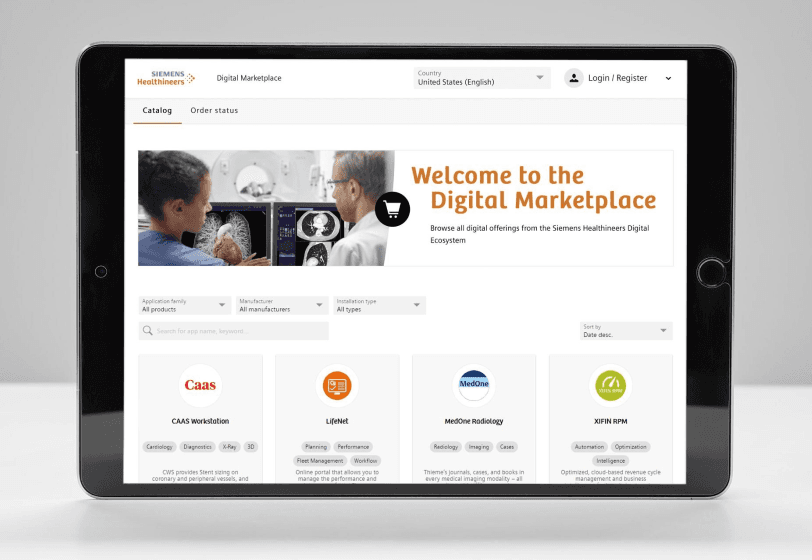
4. Managed services: Interoperability-as-a-service, where OEMs manage integration, compliance and updates on behalf of providers

Device data that once sat idle can be harnessed to drive predictive insights, personalized care journeys and outcome-based contracts. Providers benefit from seamless platforms that reduce readmissions and streamline workflows. Payers see improved cost efficiency through proactive interventions. And patients gain more control and convenience through integrated apps, dashboards and remote monitoring tools. This manifests in a number of practical use cases, including:
Oncology
Use case: Precision oncology treatment intelligence platforms:
- Integrates radiotherapy dosing, treatment plans, genomic sequencing
- Tracks outcomes and toxicity data longitudinally
- Enables adaptive treatment models based on patient response
Therapeutics
Use case: Integrated disease management platform for complex, commutable conditions:
- Cross-modality integration normalizes streams from disease-specific devices
- Multi-morbidity intelligence provides core services like therapy optimization and predictive risk alerts
- Adaptive care pathways support modular add-ons for each therapeutic vertical
In-hospital monitoring devices
Use case: Centralized patient monitoring & risk prediction platform:
- Streams data from bedside monitors, ventilators, infusion devices
- Provides a unified ICU dashboard with AI-based deterioration alerts (e.g. cardiac events)
- Generates structured datasets for outcomes research and hospital efficiency optimization
For more practical use cases and examples, download our full playbook here.
Benefits of healthcare data integration
There’s multiple benefits of solving the data integration challenge for medtech OEMs, which is why the market continues to grow. Those that cultivate a thriving healthcare ecosystem will:
- Accelerate innovation by creating unified data environments where new digital services can be built rapidly
- Diversify revenue by moving beyond hardware into subscription-based platforms and analytics-driven services.
- Strengthen relationships with providers by enabling outcome-based care and collaborative partnerships. And most importantly…
- Become AI-ready, positioning themselves to capitalize on predictive insights, clinical decision support, and personalized medicine — all while staying compliant with evolving regulations
Creating a systematic framework
The journey from device maker to ecosystem orchestrator requires a deliberate approach. It should include a basic integration stack framework:
- Data ingestion from diverse devices and sources
- A powerful integration engine to unify streams
- Centralized data warehousing for secure storage and access
- Analytics and AI layers that transform raw data into actionable insights
With this framework, medtech companies can break free of siloed data platforms and offer connected solutions that scale. The shift requires both technical execution and organizational transformation that allows for adopting agile development practices, embedding software and AI expertise and building compliance processes that keep pace with the speed of digital health.
Healthcare data integration isn’t a one-time thing, it’s the backbone of long-term healthcare ecosystem strategy.
How to build a healthcare data ecosystem
Healthcare customers are making decisions now about which partners can deliver integrated, outcome-driven solutions. For medtech OEMs who want to succeed in the coming years, it’s imperative to start tackling healthcare data integration by becoming trusted health ecosystem data orchestrators and monetizing data flows.
Learn how to achieve this, and the technology behind it, in Star’s orchestrator playbook below.