Healthcare is unreasonably expensive. On a per-capita basis, healthcare spending has increased 31-fold in the past 50 years. In 1970, the annual cost of care averaged $355 ($2,382 in 2020 dollars) per person. It’s now reached $11,172.
Consider all of the medical breakthroughs of the last few decades and regulations like the ACA that are designed to curb healthcare spending. Even with these, total US healthcare spending now exceeds $3.6 trillion, accounting for 17.7% of GDP.
Beyond unlocking medical innovations, data science reduces costs, passing on savings to both payers and patients by focusing on evidence-based outcomes, transparency and accountability. In short, the healthcare system is sick, and data science is the cure.
Get an insight-driven guide on AI in healthcare. Build better MedTech products. Deliver greater AI experiences within the healthcare system.
The dire need for value-based care
A quiet storm has been raging in the healthcare world for several years. Payers are shifting away from the fee-for-service paradigm that has always dominated healthcare towards reimbursement based on the quality of care provided, rewarding providers both for effectiveness and efficiency.
While this approach may seem intuitive, it actually goes against long historical precedent not just in the US but around the world. The fee-for-service (FFS) model effectively incentivizes the provisions of more services and treatment as payment depends on quantity, not the quality of care. Unsurprisingly, FFS is associated with higher costs while discouraging integrated care practices.
FFS is a logical approach to reimbursement. Providers should receive compensation for the services they provide. Over time, however, this practice has grown out of control and is one of the leading contributors to high costs, along with declining population health across the system today.
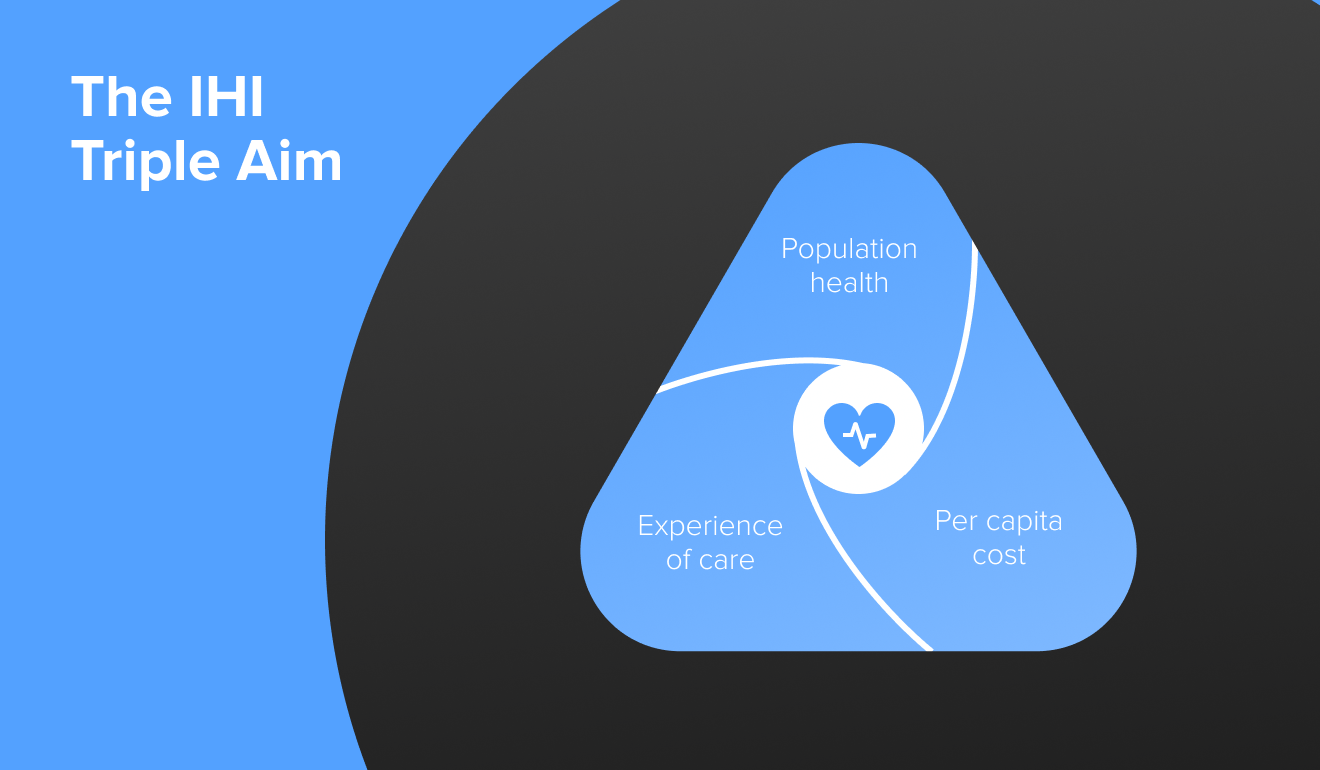
Value-based care, also referred to as evidence-based care and pay for performance, ties reimbursement directly to quality and health outcomes. As a result, it more strongly advances the triple aim through promoting better individual care, improving population health management strategies and reducing costs.
Data science in action
While 2020 will be forever known for the scale and magnitude of the challenges COVID-19 created, we are still in the midst of several endemic population health crises. Whether it's the opioid epidemic, rising obesity rates, chronic health conditions and other challenges, these population health challenges fundamentally impact healthcare costs, outcomes and success.
Data is the key to overcoming these crises. Data science allows providers to aggregate data from disparate sources to solve problems, and create and adhere to evidence-based and effective solutions built on efficiency, efficacy and transparency.
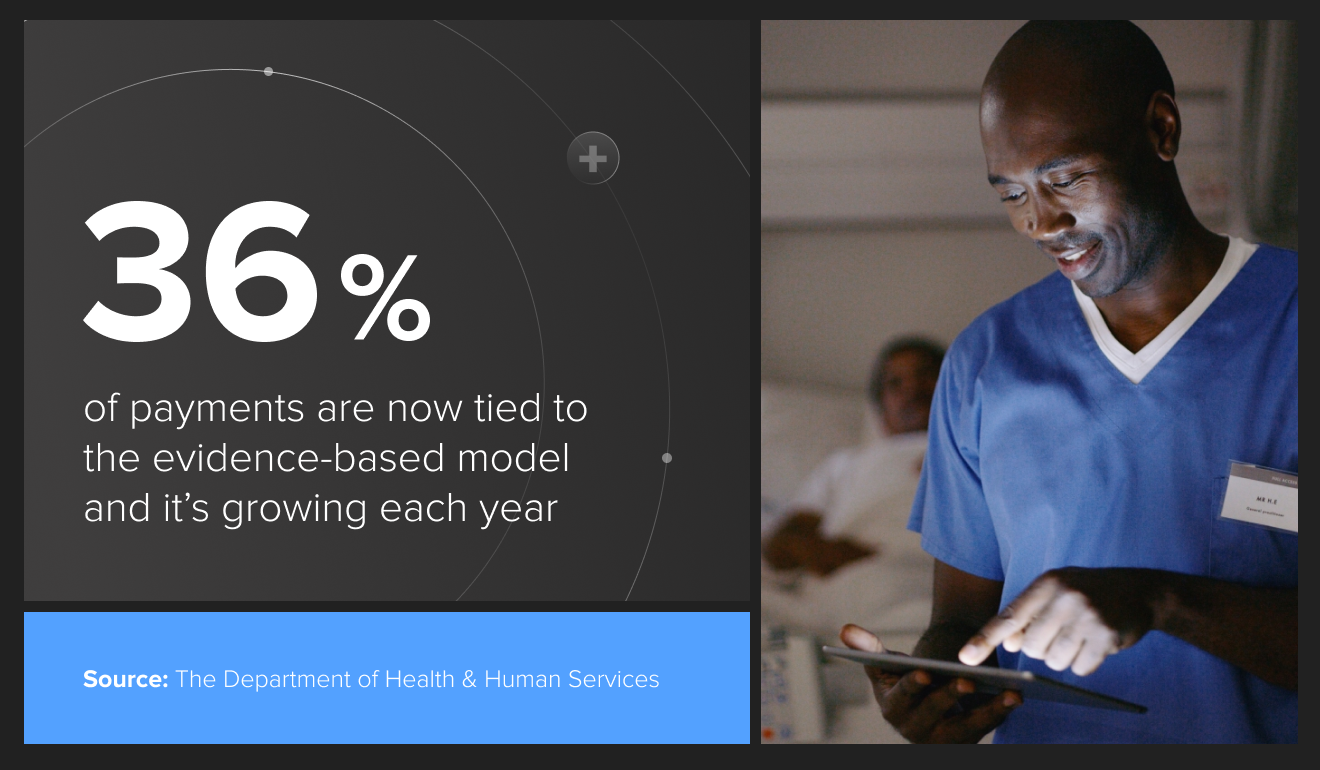
Take just one of the biggest payers out there - The Department of Health & Human Services. They have been converting their previous fee-for-service Medicare reimbursements to value-based payments over the past five years. 36% of it is now tied to the evidence-based model and it’s growing each year.
Data science is there every step of the way in this new approach. Whether it’s data analytics to track costs and payments made, upgraded health IT or establishing benchmarks for what constitutes both evidence and progress made, it’s the driving force behind the value-based care revolution.
How to put data science to work
As the shift towards value-based care continues, science becomes even more essential for validating evidence-based outcomes. Reimbursement will grow increasingly tied to outcomes, so providers need to start building data stories that prove the efficacy of treatment approaches.
To be successful, you need to understand the measure of efficacy. What are the success metrics for treating a given condition? How do you provide evidence of progress? Obviously, there is no one-size-fits-all approach. Fortunately, we're already seeing examples of successful data science applications across healthcare that shed light on these questions.
Chronic condition management has been one of these leaders in the integration of data science for the delivery of value-based care. Welldoc's diabetes SaMD BlueStar has been so well received that it has even achieved FDA-approval and CMS reimbursement.
Underneath the 50+ peer-reviewed publications, studies and compliance, BlueStar has built a strong data foundation. It specifically improves diabetes management through individualized coaching and tracking based on blood glucose levels, medication and lifestyle to improve A1C.

All of this is built on top of huge datasets and global benchmarking and cross-checking with similar research on diabetes in China and Australia. The result is a comprehensive health solution that is significantly improving patient quality of life and overall health.
There are countless other examples of data science trends in healthcare. One of the most highly regarded is Omada Health’s flagship data science-powered digital therapeutic. Omada works to improve patients' lifestyles by empowering them to track health changes and make informed decisions about their lifestyle.
Both individuals and businesses have jumped on this product because it contains the complete toolset necessary for mitigating preventable health risks. Omada is even skipping the middleman and collecting its own data directly through sensors, scales and other wearables.
From here, their solution processes this alongside user-tracked behavioral data to create highly tailored programs for each patient. Concurrently, Omada also provides personal health coaches who have deep insights into patient health and who can modify and further personalize programs over time. All of this is wrapped around a machine-learning algorithm that constantly improves as it gathers more patient data.
So far, there is no common process in place to define and set metrics that measure progress and efficacy across all disease areas and conditions. Approval and reimbursement are granted in a piecemeal and case-by-case basis that is likely to remain for the next few years.
Nonetheless, Omada has been among the first virtual providers to achieve full recognition from the CDC. By meeting CDC standards and hitting clear milestones and benchmarks, they’ve been able to work themselves into a regulatory framework through objective evidence established by a key federal health agency. Consequently, they’ve managed to secure reimbursement from payers like Blue Cross Blue Shield even without FDA approval.
Start leveraging data science now
From improving chronic disease management to predictive medicine while simultaneously making patient care more affordable and effective, data science is integral for today’s healthcare.
Three interconnected key elements are behind these changes:
- The severe need to address high healthcare costs
- Large population health crises including COVID-19, but also chronic conditions, the opioid epidemic and other challenges
- Technological advances, including artificial intelligence, machine learning and wearable sensors.
As healthcare continues to grow increasingly value-driven, industry leaders must begin to understand these changes and develop data-driven efficacy measures.
The first step to achieving success is to map the benchmarks and metrics that will provide evidence of the efficacy of a treatment plan and progress. As such, this core data will form the strategic foundation necessary for all data science projects by informing what the key requirements of a specific data set need to be.
The healthcare system may be in serious crisis, but data science improves outcomes, lowers costs and guarantees a win for all stakeholders. Start harnessing its potential now.