AI and ML are transforming healthcare. No matter where you look, it’s helping improve disease prevention, optimize patient and provider experience and increase access to healthcare services. The use of AI in healthcare technology in remote monitoring, diagnostics and software as a medical device solution has accelerated the shift from in-hospital to in-home care and decreased the burden on the healthcare system.
Artificial intelligence in healthcare is nothing new. It’s been talked about since the 1960s. But we’ve finally reached the inflection point in which we can start unlocking more of its potential. Between the awesome amounts of computational power now available and the vast array of EHR, healthcare system, IoMT and wearable data, we can begin creating and deploying AI across software-as-a-medical devices, digital therapeutics, diagnostics and many other applications.
At Star, we are incredibly excited about AI’s potential in healthcare. It’s a technology we use every day to help our clients tackle immense challenges and create new opportunities for better outcomes for everybody in healthcare. For example, we work with a UK-based company that employs AI to diagnose skin cancer. With it, a diagnosis that could take weeks to receive in the past can now be delivered almost instantly. In fact, you could test and diagnose the entire population of the UK (67 million people) in just a few days with our co-created solution.
Whether you're already in the HealthTech business or looking for a reliable partner to leverage your ideas on how to successfully release your medical device to the market, we can support you across the entire end-to-end product journey and create more value by harnessing AI technology.
AI technology is complex. But everybody can understand its potential to revolutionize healthcare. That’s why we’re going to walk you through use cases, key technical considerations, and the types of business outcomes companies can achieve by leveraging the technology. Above all, we’ll show you that AI isn’t the future of healthcare — it’s the present, and it’s already radically reshaping care delivery, prevention, administration and so much more.
Download our ultimate AI in healthcare report. Latest AI trends and insights for executives in medtech and healthcare providers
Artificial intelligence, algorithms and data: how AI works in healthcare
Anytime you hear about AI, you should be thinking about data. Data is the fuel for AI. For successful AI product development, you need a lot of high-quality data. It requires a lot of input to be trained to create an accurate diagnosis. In fact, this is one of the first questions we ask prospective clients.
Legacy healthcare businesses are sitting on data goldmines that often include images, blood tests, patient histories and clinician work ready to be put to use (with patient consent of course). Fortunately for startups, you can purchase relevant data for your intended project, but you have to be careful about its quality and source — not to mention the price!
We can go on for days about the complexities of healthcare data, including whether data is structured or unstructured — clearly defined and searchable vs. data stored in its native format.
For our purposes, we’re just going to focus on high-quality data in a broader sense because that’s just the tip of the iceberg when it comes to training AI. But first, it’s important to distinguish between traditional algorithms and artificial intelligence.
With traditional algorithms, everything boils down to either true or false. They follow “if” and “else” statements contained in a programming language. Put simply, with a traditional algorithm, you can say for sure that 2+2=4. But this dependence on predefined rules limits what they can do.
AI works differently and tends to be much more complex. There are many types of AI approaches, but we’ll focus on neural networks since they are often used in healthcare. They are assembled from neuron models where a single neuron sums input, their corresponding weights, a bias and applies the activation function which produces a value. The value is an input for the next neurons usually located in the different layers to finally produce the output values of the neural network.
With neural network AI, unlike traditional algorithms, there is no 100% certainty. Instead, it could say something like, “there is a 95% chance that 2+2=4.” If AI is well-trained and has enough high-quality input data, it can provide higher probability results that push closer to 100%.
This probability-driven approach can be better applied to the more complicated and uncertain problems which are common in healthcare. Machine learning (a subset of the wider AI domain) and its ability to solve large, complex problems across many data points is proving to be an incredibly powerful tool across a wide range of applications. With it, we can create learning models that get smarter, more accurate, and faster over time and support both clinical and non-clinical applications.
Key considerations for developing artificial intelligence in healthcare
Because the stakes are so much higher in health, selecting the right architecture, defining the software unit, verification and validation as well as risk management plan are crucial to safety, efficacy and passing regulatory body audits.
While you could write a book on each of these different aspects of AI software creation, we’ll focus on a few of the biggest considerations. For medical device product development, you have to always consider your intended use statement.
Whether your device contains an AI component for advisory and data processing versus diagnosis and treatment will significantly impact your regulatory journey. Using skin cancer again as an example, if your AI system says there’s a 95% chance a lesion is cancerous, but a doctor makes the actual diagnosis, your device can be classed at a less restrictive software safety classification.
Did you know? You can’t use all your data in one place. You’ll need separate subsets of data for AI training and validation.
On the other hand, once an AI-powered software as a medical device (SaMD) makes the actual diagnosis, the requirements get much stricter. However, with mounting healthcare worker shortages, many companies will naturally pursue product strategies based on high levels of autonomy and reduced clinician involvement. Over time, it’s even possible to imagine that a significant part of a physician's job will effectively be rubber-stamping machine-made decisions as their role morphs into that of compassionate caregiver, explainer and overseer.
Whatever solution you design, the software requirements must reflect this intended use.
Never assume 100% accuracy of the results when specifying your software requirement. Instead, define your health software AI's anticipated accuracy in terms of probability. Remember, humans seldomly have 100% diagnostic accuracy, and the regulator doesn’t expect your medical AI to have it either.

AI training and optimization
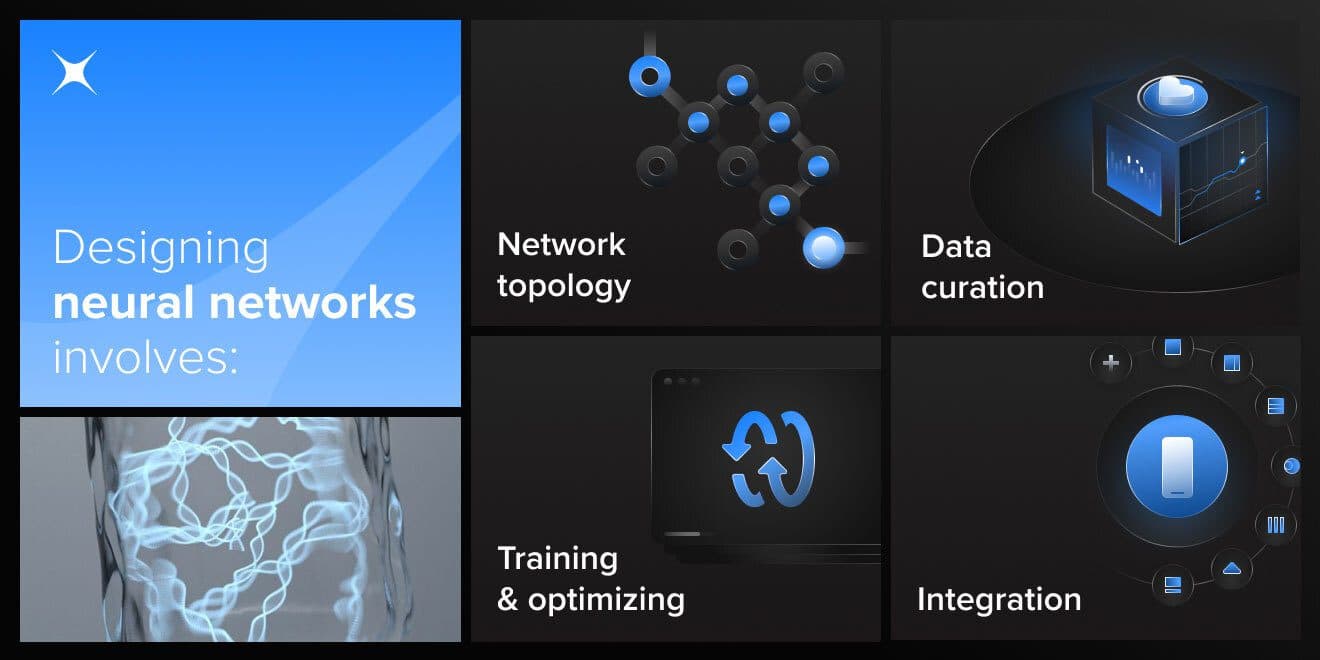
The most important part of artificial intelligence in medicine software development is designing, training and neural network optimization. During this phase, you will have to select or design a neural network that is the most suitable for the problem you are going to tackle.
Knowing which you’ll choose involves:
- Network topology – What kind of network will work best for your problem? Will you go for any of the well-known classes like Convolutional Neural Networks (CNN), Recurrent Neural Networks (RNN) or Long Short-term Memory Networks (LSTM)? Does your problem require developing more sophisticated topologies (e.g., GRU, VGGNet, ELM), or even your own proprietary neural network topology? If all this is starting to sound like a foreign language to you, don’t worry. That’s the type of help we offer here at Star.
- Data curation – This is even more important than your network configuration. This step aims to prepare data that will be used to train your neural network. You should have both the input data and the expected results prepared. The more reliable your data set is, the higher the chances of training and optimizing the AI model to fit your needs. Be sure to protect your data. Without proper security, a competitor can use your data to come up with their own AI configuration. You will also need that data later for verification and validation of your medical device and in clinical trials.
- Training/optimizing – Now it is time to train your network, optimize and keep repeating this process over and over again until you fall within the probability expectations specified in your software requirements. It takes time, computing power, and knowledge to train your network, polish learning data, modify neural network topology, and re-evaluate learning processes. To cut costs in this phase, we usually train AI on physical HW supported by GPUs (graphics processing units) or in the cloud.
- Integration – Remember, AI is just one component of your overall solution. You have to integrate your AI software unit with the rest of the system architecture. The interfaces should be precisely specified, as quite likely your AI will be released quite often. Thanks to carefully selected interfaces, your AI can be both forward and backward compatible from a product life cycle perspective. Equally important are the questions of scalability. For example, operating an EC2 Elastic GPU (cloud-based GPU resources) comes with a hefty price tag. If you design and integrate your solution with horizontal scaling, you can save costs and take advantage of a pay-as-you-go approach.
The business advantages of adopting AI into your healthcare software products
In addition to the benefits for patients and providers that AI creates, it also has numerous advantages for businesses. While some AI solutions in healthcare may be costly upfront to develop, their long-term profitability and cost-reduction are unparalleled. In 2021 alone, AI has saved $52 billion in the healthcare sector. And it gets even better. Thanks to hardware improvements, operational costs go down each year.
If we look at even just a handful of AI use cases, it's easy to see why. For example, let's say you create an AI-fueled SaMD that can diagnose disease in just a few seconds. Some companies get paid per diagnosis, and this alone can add up quickly.
Simultaneously, we are talking about efficiency. That's why some of our favorite healthcare AI companies might not be the most famous yet, but they’ve already had a significant impact at every stage of care. For example, voice assistants are a popular solution for many of our clients. Using natural language processing, they can understand speech input and directly transcribe medical data to an EHR. As a result, this has the potential to reduce the administrative burden on clinicians, improve clinician-patient interactions, and reduce financial pressure on healthcare enterprises.
Likewise, implementing AI in healthcare is equally advantageous for non-clinical applications. Conversational user interfaces, including relatively simple chatbots, can help with appointment scheduling, medication reminders and just generally increasing accessibility to healthcare.

Looking ahead: the future of AI in healthcare
We are only at the beginning of the AI in healthcare era. As we look into the next few years, we see so many exciting examples of AI. We see huge potential in accelerating drug development, digital twins and enhancing clinical decision support.
And this barely scratches the surface of what AI will be able to do. Discover more in this expert report from HLTH 2021, in which Star’s HealthTech Practice recaps the most impactful trends and technologies shaping medicine today.
While you’re at it, see Star HealthTech in action. Dig into this case study from our recent collaboration with the Design Institute for Health in which we envision the future of healthcare. It’s a bold, design-driven look into four different health scenarios that showcases our endgame approach to problem-solving.
Image sources: sites, bangkokinternationalhospital